Building medical electronics isn’t just a technical challenge. It’s a regulatory crucible.
You’re not just designing for performance. You’re designing for inspection. For traceability. For validation of critical components in your medical devices.
Whether you're building a wearable Class II diagnostic device or a life-sustaining Class III device, the FDA doesn’t care how brilliant your prototype is if you can’t prove how—and why—it was built. This involves ensuring that every step is traceable, particularly in compliance with the standards of industrial manufacturing companies.
This isn’t a sidecar function. It’s core to your engineering workflow. Here’s how to bake compliance into your product development process—without losing momentum, blowing your budget, or ending up in submission hell. Embracing proactive strategies and agile methodologies can significantly aid in this regard.
1. Your classification determines your roadmap. Know it early.
Designing before classifying is like writing code before defining your inputs.
Class I? You might be fine with a solid QMS and basic documentation.
Class II? You’re likely heading into 510(k), ISO 14971 risk management, and full Design Controls under 21 CFR 820.30.
Class III? Buckle up for PMA, clinical trials, and zero tolerance for untracked decisions affecting your component supply chains and critical components.
Strategy tip: Engage a regulatory consultant before you build. We’ve seen founders burn a year treating a Class II like a Class I—only to restart the entire V&V process after failing submission.
2. Design controls are the real product
If it’s not documented, it didn’t happen.
Design Controls aren’t just FDA red tape. They’re the audit-proof breadcrumbs that trace how you got from “here’s a user need” to “here’s the validated, functioning device.”
You’ll need:
- User needs → Design inputs → Design outputs
- Verification, validation, reviews
- Controlled change orders
- A complete Design History File (DHF)
Pro tip: Start your DHF during EVT. Waiting until PVT? You’ll be retrofitting paperwork—and the stress of that is exponential.
3. Your prototype is a compliance artifact
Most teams treat prototypes as throwaway builds. In MedTech, your regulators don’t.
Every early build is a preview of your production process. And a prototype without documentation is a liability, not a milestone.
Include in every prototype:
- Version-controlled BOMs
- Schematics with change logs
- Test reports linked to firmware versions
- Photos, inspection records, serial numbers
- Notes on EMC/ESD pre-compliance tests
Think of your alpha build as Exhibit A in your submission dossier. Build it like it’s going on trial.
4. Risk management isn’t a phase. It’s a lens.
Under ISO 14971, risk is not something you “check off.” It’s a living system.
From your first schematic, you’re making safety decisions. A weak voltage regulator can cause thermal drift. An intermittent UART line can cause bad dosing logic.
Good engineering means:
- FMEAs at system and component levels
- Software hazard analysis (not just feature testing)
- Risk mitigation embedded in firmware and hardware (e.g., watchdog timers, redundant reads)
Your EMS partner should understand this. If they don’t speak FMEA, find one who does. Industry leaders recognize the importance of having partners who can speak the same technical and regulatory language.
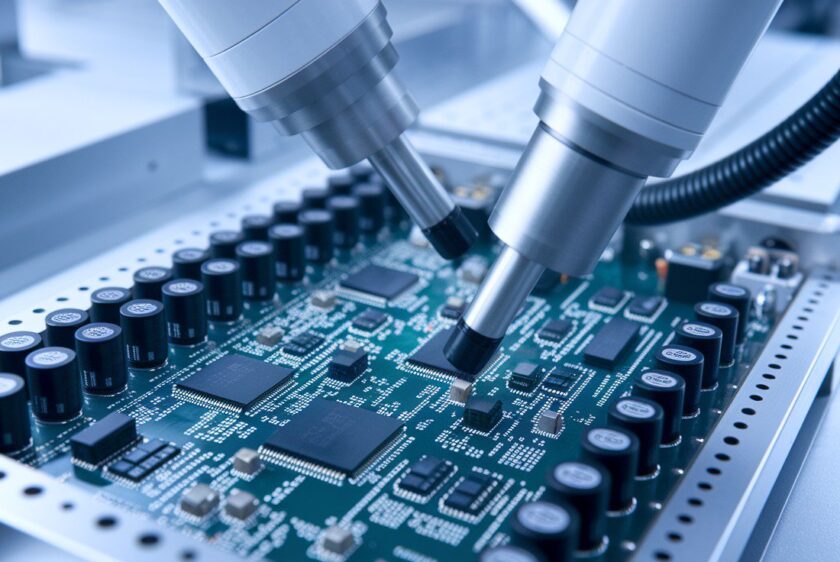
5. Your EMS is now part of your regulatory file
Your EMS is part of your FDA story. A legacy equipment manufacturer (LEM) with deep industry knowledge can be a critical alliance.
If they’re not ISO 13485-certified or don’t know what a DHR is, that’s not a vendor—it’s a regulatory risk. Multidisciplinary sourcing strategies and strategic partnerships with component suppliers can help mitigate risks.
At EST, we’ve supported customers through:
- Class II and III builds
- Cleanroom and sterile packaging
- FDA and notified body audits
- Maintaining QMS integrity across product lifecycles
What to look for in a partner:
- ISO 13485 certification
- Lot-level traceability
- Electronic traveler systems
- Controlled document management
- Validated rework and inspection processes
If they “don’t normally build for medical,” don’t be their test case.
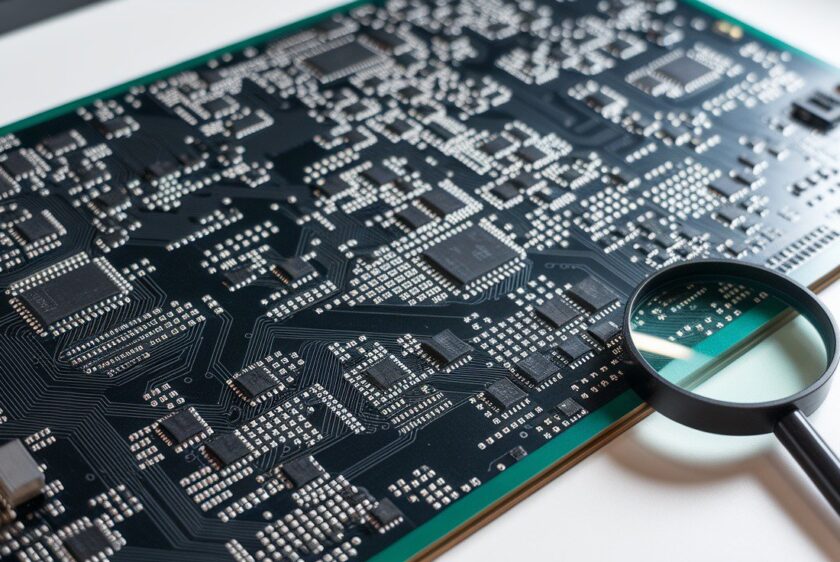
6. Traceability isn’t a feature. It’s an insurance policy.
When (not if) something goes wrong in the field, the first question will be: which lot? which board? which part?
You should be able to answer in seconds:
- What supplier the part came from
- What lot and shift built the board
- Who inspected it
- What firmware version it shipped with
At EST, we track this across every stage. No MES required—we use barcoded inventory, AVL-controlled BOMs, and serialized builds to keep it clean, lightweight, and audit-ready. This allows for efficient supply chain management across the entirety of the product lifecycle.
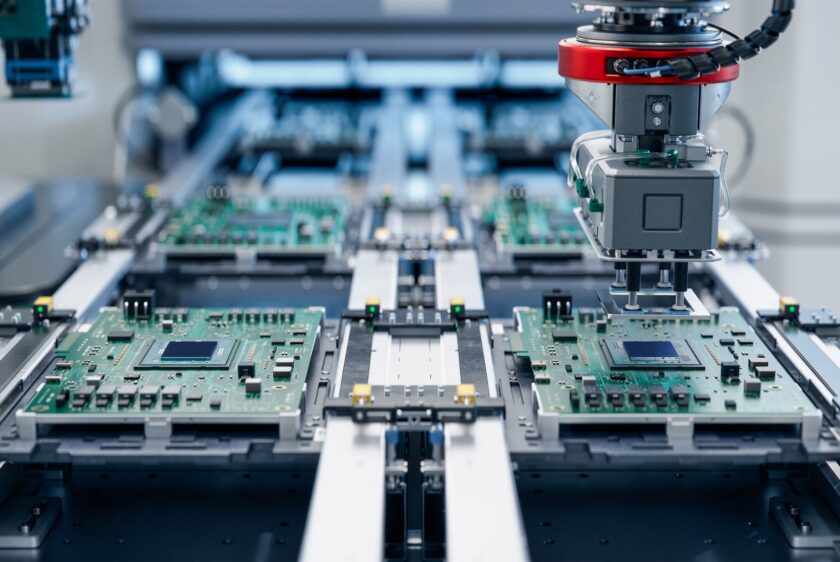
7. Design for test. Or prepare to regret it.
You can’t validate what you can’t test. And the FDA doesn’t believe in “just trust us.”
Your board should include:
- Test points on every power rail and critical node
- Built-in self-test routines in firmware
- JTAG or debug headers (yes, even in production)
- Clear separation of analog/digital grounds and HV/LV domains
On the floor, that enables:
- Flying probe or ICT
- AOI and in-process inspection
- Functional hardware/firmware testing
Bonus: All of these generate logs, which you can use to validate your process control during audit.
8. Medical-grade components where it matters
The FDA won’t demand medical-grade everything—but your notified body might. So might your future acquirer.
Where it counts (power, sensing, actuation), spec:
- IEC-certified components
- Long lifecycle SKUs
- Hermetically sealed or biocompatible parts
And don’t forget to track:
- Country of origin
- RoHS/REACH status
- Conflict mineral disclosures
A single off-spec capacitor can derail your entire validation plan. Source smart, document everything to ensure a resilient future for your products.
9. EMC and ESD testing are not optional
It’s shocking how often this is skipped until the end.
Most Class II and III devices will need:
- EMC: IEC 60601-1-2, EN 55011
- ESD: IEC 61000-4-2
- Electrical safety: UL 61010, IEC 60601-1
Design with this in mind:
- Add TVS diodes on all I/Os
- Use filtering on USB/data lines
- Separate grounds with intent
- Keep clearance/creepage specs tight
Do pre-compliance testing during DVT. It’s cheaper to tweak a layout than fail a full test chamber at the 11th hour.
10. Documentation is the product
Compliance isn’t a checklist—it’s a narrative. Your DHF, DMR, and DHR should tell a story a regulator can follow:
- Here’s what we were building
- Here’s how we proved it worked
- Here’s how we built it again (and again)
- Here’s how we know every unit shipped is traceable
If any of that lives in your engineer’s head or a shared folder called “final_final_THISONE_v3,” you’re not ready.
Final thought: Compliance is a design constraint—not a bottleneck
The most successful MedTech teams don’t treat compliance as a barrier.
They treat it like a protocol: consistent, rigorous, agile, and designed to build trust.At EST, we’ve helped VC-backed startups and Fortune 100s go from napkin sketch to 510(k) without burning time or trust. Not by cutting corners—but by cutting ambiguity.
The engineering is the easy part. Proving it to the FDA? That’s where the real build begins.